Erika Zar, 45, tried many different kinds of birth control before she settled on her current one. “Most of them seemed to amplify my mood shifts,” she said. The birth control pills that she tried lowered her sex drive and made her depression worse, and the vaginal ring made her so “ragey” that she only lasted seven days with it.
After two emergency surgeries to treat her endometriosis, Zar was prescribed a hormonal intrauterine device (IUD) to help control the disease — and she’s still using one over a decade later. After years of trial and error, she’s happy to have found a form of birth control that meets her unique needs.
With so many birth control options available, it can be hard to know which one is right for you. Some women prefer non-hormonal birth control because they worry about side effects from hormonal options, or they have health conditions that make hormones unsafe. Others might like the convenience of hormonal birth control or have health conditions, such as endometriosis (like Zar) or painful cramps, that are improved by it.
Being informed may help a woman choose the right birth control for her
Nearly half of all pregnancies every year in the United States are not planned, yet around one-third of women who could become pregnant don’t use contraception. Why might a woman who doesn’t want to become pregnant not use birth control? Reasons vary but may include lack of access or knowledge, infrequent sex or concerns about how their health will be affected.
When it comes to helping women decide to use birth control, information often plays an important role. One large study found that teenage girls who had thorough sex education before becoming sexually active were more likely to use some type of birth control when they had sex.
Understanding the differences between hormonal and non-hormonal birth control can help you make the best choice for your body — and your lifestyle.
Non-hormonal birth control offers on-demand protection without hormone side effects
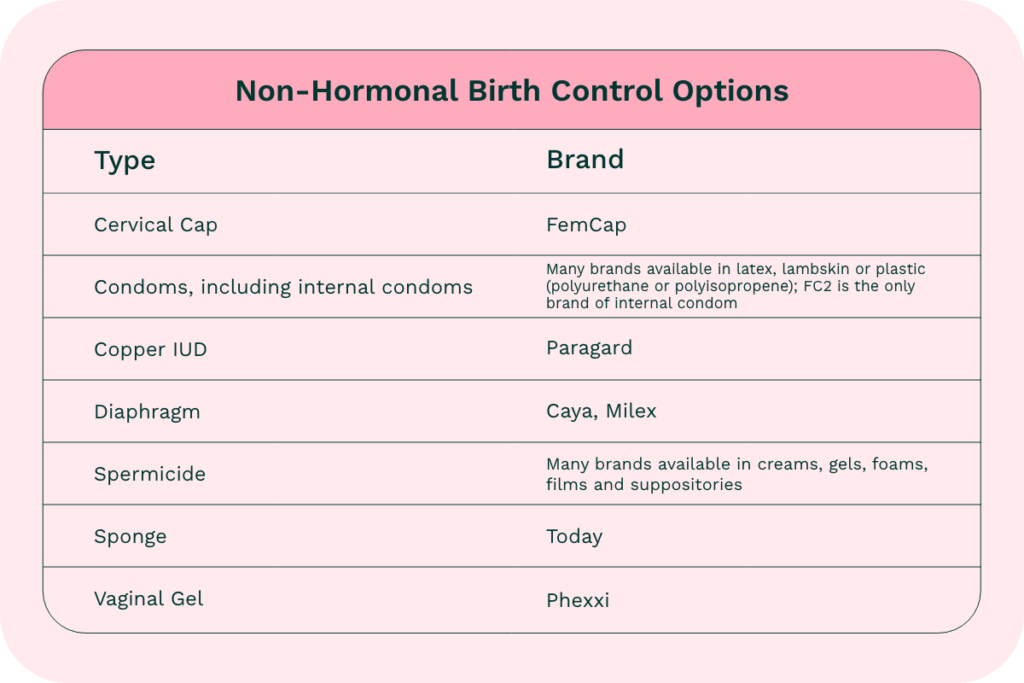
Non-hormonal forms of birth control include condoms, sponges, diaphragms, cervical caps, non-hormonal copper IUDs, spermicide and the acid-based vaginal gel that was recently approved by the U.S. Food and Drug Administration (FDA). Rather than making hormonal changes, these methods prevent pregnancy by forming a physical barrier that keeps sperm from entering the uterus or creating an environment that prevents sperm from successfully fertilizing eggs.
Non-hormonal birth control often appeals to women who want control over when they’re protected, according to Dr. Nisha Verma, a family planning fellow and OB-GYN at Emory University. This might include women who only need protection from pregnancy once in a while or women who prefer to choose their birth control method in the moment instead of using a long-acting form. Non-hormonal birth control can also be ideal for women who don’t want to override their natural menstrual cycle or put something in their body every day. “People like that it’s something they can use just when they want it,” Verma said.
Women who have health conditions that prevent them from taking hormonal birth control or have experienced (or are afraid they may experience) side effects from hormonal birth control — like weight gain or lowered sex drive — may also seek out non-hormonal options for preventing pregnancy.
Condoms are a form of non-hormonal birth control that offer the added benefit of preventing sexually transmitted infections (STIs) and HIV. It should be noted that only latex or polyurethane condoms (not lambskin) offer this protection.
Hormonal birth control provides continuous protection and other health benefits
For women who want their birth control to be “on” all the time, there are many hormonal options that provide continuous protection against pregnancy. Birth control pills, patches, shots, and vaginal rings are considered short-acting forms of hormonal birth control, while hormonal IUDs and implants can provide protection for many years. Both short- and long-acting hormonal birth control methods work by releasing hormones that change the body’s chemistry to prevent pregnancy.

According to Verma, many women are drawn to hormonal birth control because it can be used for more than just pregnancy prevention. Some women with heavy or irregular periods — including those with conditions like fibroids, endometriosis or polycystic ovary syndrome (PCOS) — use hormonal birth control to regulate their cycles or reduce ovarian cysts, while others like the option of not having a period at all. Verma adds that women dealing with hormone-related health issues like acne or mood swings may also turn to hormonal birth control for help.
But hormonal birth control isn’t without drawbacks. “There are safety concerns, particularly with birth control methods containing estrogen,” Verma said. For people with certain health conditions like migraine disease, high blood pressure, breast cancer or a history of blood clots, Verma said, hormonal birth control containing estrogen may not be safe.
There is no “best” birth control
Verma says that healthcare providers have changed the way they talk to their patients about choosing birth control. “When the long-acting reversible contraceptive methods came out, there was a lot of excitement about them — and a lot of pushing of these methods,” she said.
But these days, Verma and her colleagues have largely shifted their approach toward talking to women about all their birth control options (both hormonal and non-hormonal), and then helping them decide which one best fits their lifestyle.
What works for some might not work for others, Verma said. “No one can tell you what’s doable for you.”