Nearly 360,000 service members were diagnosed with a sexually transmitted infections (STIs) from 2013 to 2021, and more than a third were women, even though women only make up less than 20% of the U.S. military.
Some studies have shown that STI rates among military personnel are as much as seven times higher than the general population.
And women in the U.S. military are diagnosed with STIs at higher rates than the general population, as well as higher rates than their male counterparts.
Between 2019 and 2021, military women were diagnosed with chlamydia three times more than male troops; gonorrhea 1.4 times more; genital herpes, four times more; and HPV, nine times more, according to data published by the Department of Defense (DoD) Armed Forces Health Surveillance Division.
But in that same time frame, diagnostic rates for four of the five most common STIs (chlamydia, gonorrhea, herpes and human papillomavirus [HPV]) declined slightly for military women, according to the DoD report.
This is a step in the right direction for protecting the health and fertility of servicewomen and service members with female biology, and ensuring that the armed forces are able to continue to provide national security.
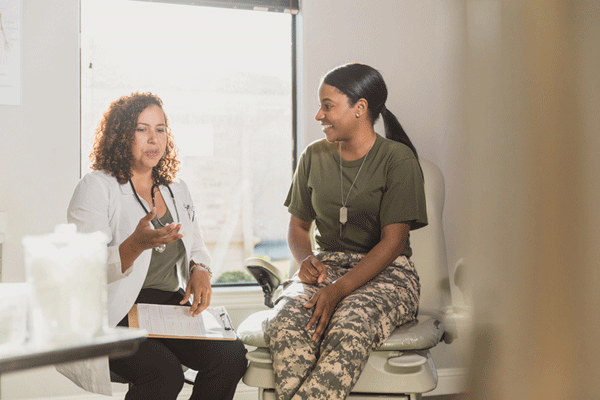
“If [a service member] is not treated for an STI, it definitely affects readiness, especially with women. It affects our fertility. It affects mental health and how we feel. If [troops] aren’t ready to go and the rest of their unit is moving on, it’s a problem,” said Ada Stewart, M.D., a family physician and colonel in the U.S. Army Reserves.
Reasons for high rates of STIs in the military
The number of STIs diagnosed in the U.S. military has gone up and down over the past decade, but has increased overall, just as it has across the country.
It could be easy to link high rates of STIs to the fact that when compared to civilians, young service members are more likely to engage in high-risk behavior, such as having sex with multiple partners, not using condoms and binge drinking. In fact, in a 2018 DoD survey of active-duty troops, nearly 35% of responders said they had sex with a new partner without using a condom, nearly twice the rate reported in 2011.
But additional factors may be at play when it comes to the high diagnostic rates for STIs among service members with female biology. According to Stewart, women may be diagnosed more because they have more regular medical screenings.
“Think about it — women have mandatory Pap [tests] and yearly screenings that men don’t,” Stewart said.
Lt. Karli Woollens, a family medicine specialist at the Navy Medicine Readiness and Training Command in Bremerton, Washington, agreed.
“They are more likely to be screened and therefore diagnosed with STIs due to recommended screening programs for all asymptomatic sexually active young women and pregnant women,” Woollens said in a media release.
Differences with the general population
In the U.S. military, chlamydia is the most often diagnosed STI, seen more than the other four most common STIs — gonorrhea, syphilis, herpes and HPV — combined, according to the DoD report. But chlamydia is not the most common STI in the U.S. overall. HPV is.
Although HPV is the most common infection, its rates have been on the decline, including among U.S. military personnel, largely because a vaccine was approved for use in women in 2006 and men in 2010.
According to the report, non-Hispanic Black troops and unmarried service members are diagnosed with HPV at higher rates than other members.
Younger service members, especially junior enlisted personnel, were diagnosed at higher rates than all other ranks from 2013 to 2021 for four of the five infections — chlamydia, gonorrhea, syphilis and herpes — and junior officers had the highest rates of HPV diagnoses.
High rates of STIs indicate a need for education and prevention, Stewart said.
Education and prevention
Young people who join the U.S. military have high rates of STIs even before starting their service. This may be because certain factors that come with increased risk for STIs, such as younger age, high school vs. college education, living in certain areas with high rates of STIs, and even certain races are common in military recruits. But the military does provide opportunities for health screening, although these screenings differ by gender. Women receive annual gonorrhea and chlamydia screenings, while men are only screened for HIV.
Having consistent standards for screening, testing, treatment and reporting could lead to decreases in STIs. And focusing on screening across the board — for men and women — can help reduce the stigma associated with seeking medical care for sexually transmitted illnesses, according to Stewart.
“Discrimination is a real fear. There is a stigma of the command, the higher-ups, finding out, or servicewomen don’t want to be pulled out from a mission because they’ve got an issue,” Stewart said.
“We see [disparities of care] in the military, not only through hierarchies — officer versus enlisted — but also with race. Most of it is more or less attributed to implicit biases — unconscious biases one may have — and cultural differences. We need to address education and assure there is a more diverse workforce within the military and within the military medical ranks.”
Military personnel come from a variety of backgrounds and cultures, Stewart noted, and what’s accepted for some age, ethnic and religious groups may not be the norm for others. Should across-the-board sex education be mandatory for all recruits and officer candidates? Stewart said the services are often limited in how much they can educate, given time constraints as well as political discourse.
One thing she believes, however, is that military women should be educated to know that they have power over their own bodies.
“We need to make sure women have the ability to be powerful and negotiate condom use with their male partners,” Stewart said.
According to Stewart, education and training needs to be done on a national level, beyond the military.
“There needs to be increased education; we need to recognize bias and have cultural competency.”